Alternative Systems
This track of Zurich Heart aims at disruptive innovations and technologies to facilitate radically new artificial heart designs and assist device technologies.
Soft Artificial Heart
Prof. Wendelin Stark (ETH)
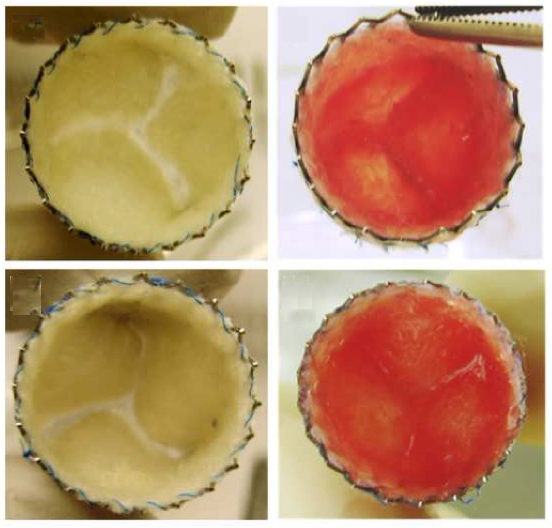
We investigate the development and use of soft robotic pumps for heart transplantation. Our goal is to develop a soft Total Artificial Heart (sTAH) which imitates the heart in its geometry and pumping mechanism. Through this we hope to address the critical shortcomings associated with the long-term performance of current mechanical circulatory support devices.
In our previous research, we have demonstrated the utility of scalable manufacturing processes to produce sTAH. The third generation of sTAHs were produced from silicone and rubber by injection moulding. Improved pumping performance and durability was measured.
In the next stages of the project, we will modify the design to improve durability and implantability of the sTAH. In addition, we aim to mimic the more complex functionalities of the native heart, for example, the Frank-Starling mechanism. Finally, we are in the process of investigating fully implantable driving solutions.
LONG-TERM INTEGRATION OF VADS – CHALLENGES AND OPPORTUNITIES
Lack of long-term hemocompatibility of artificial materials at the luminal surface of VADs leads to thrombosis at the blood to surface interface. This in turn increases the risk of thrombogenic events triggered by implant materials. Hemocompatibility of such cardiovascular implants can be improved by coverage of the luminal interface with living endothelial cells. Hence, a mature endothelium at the luminal interface that is in contact with blood can provide protection from thrombus formation and subsequent adverse events. However, the endothelialization of blood pumps remains largely unexplored due to the non-physiological hemodynamic conditions created by the active implant. In addition, the harvesting of a sufficient number of healthy autologous endothelial cells from cardiovascular patients may prove challenging. Biological senescence in those autologous cells affects the cell’s function and ability to reconstitute a functional monolayer.
Surface nanoengineering for improved hemocompatibility
Prof. Edoardo Mazza (ETH), Prof. Volkmar Falk (DHZB / ETH), Dr. Aldo Ferrari (ETH), Dr. Costanza Giampietro (ETH / Empa)
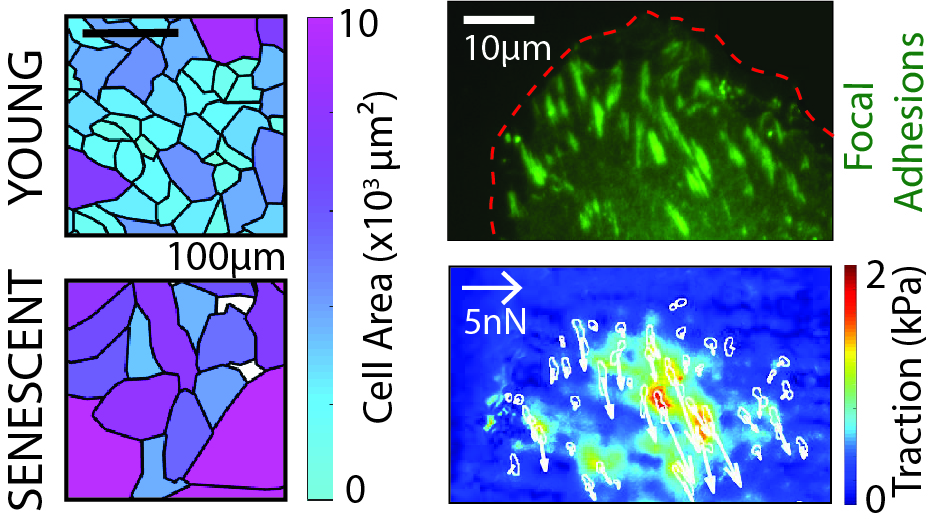
The use of topographic surface modifications to promote healing and demote infection is among the expertise of the Laboratory of Thermodynamics in Emerging Technologies (Prof. Poulikakos). The available library of surface geometries as well as new customized topographies are used for the optimization of cell ingrowth up to the formation of a confluent and functional endothelium on the target surfaces (i.e. the process of endothelialization). The group is additionally studying the mechanical properties of senescent endothelial cells with advanced force microscopy technologies.
Free-form patterning technology to support endothelialization
Prof. Edoardo Mazza (ETH), Prof. Volkmar Falk (DHZB / ETH), Dr. Costanza Giampietro (ETH / Empa), Dr. Aldo Ferrari (ETH)
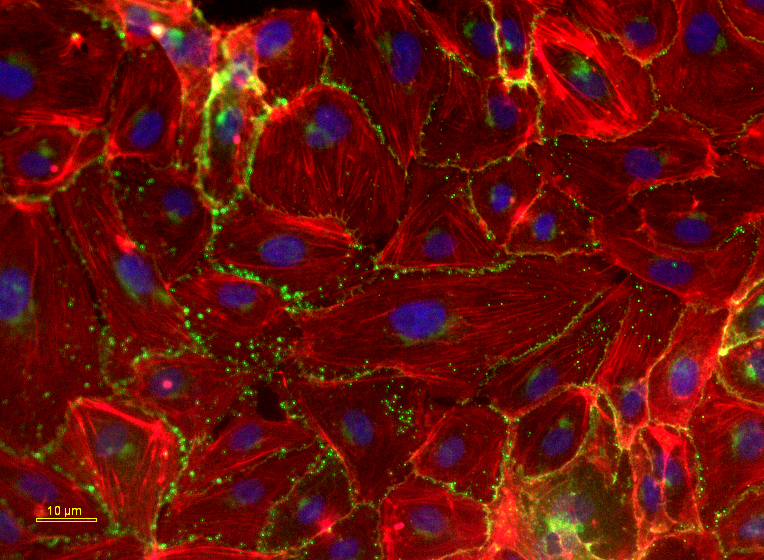
The group of Prof. Mazza and Dr. Giampietro has devised a free-form patterning method introducing arrays of microscale wells on the surface of a biocompatible silicon layer that supports the generation of mature human endothelial monolayers and their maintenance under disturbed dynamic changes. The applicability of this method to non–planar and complex surfaces, that are characteristics of the novel VADs, has been successfully demonstrated.
Towards the rejuvenation of senescent endothelial cells
Prof. Maximilian Emmert (DHZB / UZH), Prof. Edoardo Mazza (ETH), Prof. Dimos Poulikakos (ETH), Prof. Volkmar Falk (DHZB / ETH), Dr. Costanza Giampietro (ETH / Empa), Dr. Aldo Ferrari (ETH)
The group of Prof. Emmert at the German Heart Center in Berlin has investigated the ability of engineered surfaces to rejuvenate endothelial cells obtained from old donors, limiting or reverting the replicative and metabolic decay typical in these cells. The promising protocol may provide a simple solution to donor cell paucity, allowing the rapid expansion of cells in vitro, with optimal functionality for the re-establishment of a fully mature and protective endothelium.
Hyperelastic Hybrid Membrane for Biomimetic Blood Propulsion (completed project)
Prof. Edoardo Mazza (ETH), Prof. Paolo Ermanni (ETH), Prof. Stephen J. Ferguson (ETH), Prof. Simon P. Hoerstrup (UZH), Prof. Katharina Maniura (Empa), Prof. Mirko Meboldt (ETH), Prof. Dimos Poulikakos (ETH), Prof. René Rossi (Empa), Prof. Viola Vogel (ETH), Prof. Karin Würtz (ETH)
The aim is to generate a highly deformable hybrid membrane consisting of a synthetic substrate covered by an endothelial cell layer. This bio-composite material system will integrate a living biological layer into a mechanical device. It could form the basis of a 100% haemocompatible blood pump. For this application, the hybrid membrane is required to resist cyclic deformation and shear stresses from blood flow. Ensuring long-term integrity and functionality of the endothelium attached to the highly deformable substrate exposed to flow represents the major challenge of the new system. Several approaches are explored ranging from multi-layer tissue engineered constructs, to electro-spun scaffolds, to topography optimization and cell binding protein inclusions. The design of the pump is optimized in order to minimize mechanical loading of the hybrid membrane.
Tissue-Engineered Hybrid Heart Valves and Interfaces (completed project)
Prof. Simon P. Hoerstrup (UZH)
Tissue engineering technologies with human cells aim at the in vitro creation of novel living heart valves with repair and regeneration capacity. Such living valves will be designed to approximate native heart valves as to biomechanical performance and physiological surfaces.
To improve the integration of heart assist devices into the host organism, tissue engineering technologies will be used to create more physiological device-to-tissue interfaces at the level of vascular connection (engineered vascular grafts) and device to body cavity interface (engineered pericardium). Novel in situ tissue-engineered methodologies using endogenous cellular repopulation strategies will be a particular focus.